The bill to fly Jim Hopkins’ dying son Joey from a hiking accident to a hospital was “ridiculous,” Hopkins recalled, north of $35,000. Also outrageous, he felt, was that Joey’s insurance company, Blue Cross Blue Shield of Georgia, simply refused to pay.
The result: The air ambulance company came after the patient for the money. In this case, Joey’s estate.
It’s a trend. Surprise bills sent to hospital patients who thought they were fully insured are increasingly rampant. And some of the most expensive bills are going to the most critical patients, those who were put on air ambulance flights. Lawmakers in Georgia and in Washington say they want to stop it.
Recent events show progress but also raise the question of whether they will succeed.
President Donald Trump in May gave the issue momentum with a press conference calling for an end to surprise bills.
A provision in a U.S. Senate measure that has passed a key committee last month would prevent such air ambulance bills. But air ambulance companies say insurance allies sneaked a low-balled price proposal into the legislation that would bankrupt them. The proposal now faces resistance in that chamber.
A key U.S. House committee, meanwhile, has passed a compromise that would tackle surprise billing in general. That one doesn’t stop surprise billing for air ambulances, though.
Everyone from lawmakers to insurers to air lift companies maintains that they want to get the patient out of the middle of the fight.
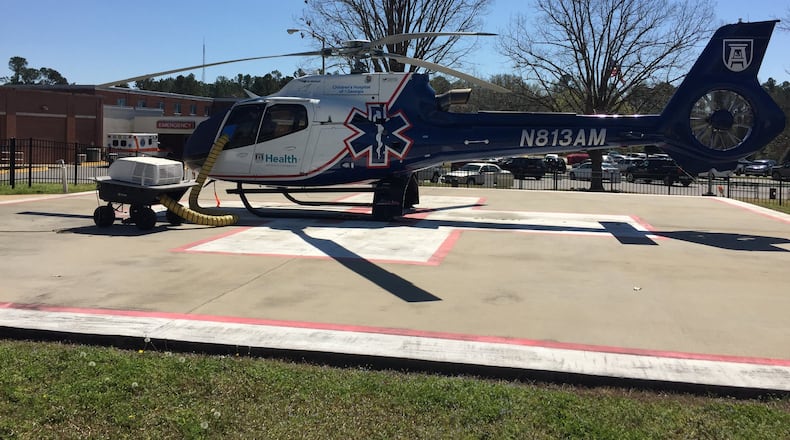
“I don’t believe a person should have to be concerned with how they’re going to pay when a physician orders a flight,” said Seth Myers, the president of Air Evac Lifeteam, which operates from 12 locations in Georgia including one near Atlanta in Snellville. “And after whatever bad thing has happened — this is a travesty for them.”
A growing problem
Surprise bills come when a properly insured patient goes to a hospital, and then it turns out his or her insurer didn't have a contract with some of the individual doctors or medical services connected to the hospital. If the service provider has no agreement on a price with the insurance company, it can send the patient a separate bill, and also set whatever price it thinks it is owed.
Insurance companies by law are supposed to cover emergency visits regardless, but sometimes they dispute the bills.
Air ambulance bills are some of the worst. The prices are huge, and estimates say more than half of rides in the U.S. on air ambulances are not in the passenger's insurance network.
The service is critically important to rural areas, where a highly skilled trauma facility, stroke center or neonatal care unit is rarely a short drive away. Rural hospitals are closing, too, meaning that there are fewer places to stabilize patients before transfer to urban areas. “If they make it where they cannot maintain their helicopters, that would hurt rural Georgia,” said Monty Veazey, a lobbyist for rural hospitals.
The trouble is agreeing what that fair price is.
Flying Joey Hopkins 39 miles in his helicopter ambulance cost $244 per mile, or $9,516, according to his bill. It also cost $719 for oxygen, $658 for his blood infusion, $255 for other supplies, and $677 for an injection gun to push fluid directly into his bone when there wasn’t time for an IV. Costs for the wait time and a night call add-on added $463.
Those were just details, though, following the company’s base charge for making a night flight call: $22,870.
The company wasn’t Myers’, but he said that total bill of $35,000 makes sense.
“There is a cost of readiness,” he said. The patient’s not just paying for the gas and supplies, he said, but for what it cost for all those people and supplies to be ready and waiting for him 24 hours a day. “We have a nurse, a paramedic, a pilot, a base — in a rural area,” Myers said.
In addition, the companies have already given up on getting full payment back from Medicare or Medicaid, which reimburse a fraction of the cost; and given up on getting anything at all from uninsured passengers. Therefore, the business model expects to make up those losses by charging insured patients even more. That’s the business model of most medical providers, in fact, from air lifts to hospitals to doctors.
Insurance companies don’t take that lying down.
Last month the lobbying group America’s Health Insurance Plans wrote to Congress that emergency health care providers engaged in price gouging. The insurers say air lift companies who aren’t in their networks should be forced to accept a price level that others in the area did accept.
“Those are fair, locally negotiated market benchmark rates,” said Kristine Grow, a spokeswoman for the group. “It’s hard to understand why or how such rates would be too low.”
Ambulance carriers say that sometimes the insurers simply refuse to contract, so that they can dispute the bills altogether.
Legislating a price war
The Senate bill may have flaws, but it would prevent surprise bills from going to patients. Insured patients would pay their policy’s normal co-pay or deductible and then walk away.
Over in the U.S. House, the bill that passed the Energy and Commerce Committee to stop surprise billing left air ambulance companies out of the ban. That bill calls for a study on the costs of the service that could then lead to legislation. Some legislators hope to add more teeth to it before it comes up for a final vote.
Both insurers and air ambulance companies say that though they’re fighting over what price to pay and who decides, getting patients out of the fray is their goal.
U.S. Rep. Buddy Carter, a Republican from Pooler who sits on the House committee, says surprise billing is one of the few issues he thinks can win bipartisan compromise right now. “People want something done,” he said.
He’s still not sure what will happen with either bill if they get a vote or reach the other chamber, though.
Jim Hopkins doesn’t care whether insurance companies win the day or air ambulance companies do. All he knows is the bill ought to be fair and fairly paid. Joey’s air ambulance bill was the last thing Blue Cross, now known as Anthem, finally agreed to pay, after Hopkins threatened to sue.
“First responders made that call” to bring in the helicopter for Joey, Hopkins said. “And you have to rely on their judgment or the whole system caves. And then you wind up with chaos — which is what we have now.”
Stay on top of what’s happening in Georgia government and politics at www.ajc.com/politics.
About the Author
Keep Reading
The Latest
Featured