Georgia EMS crews near ‘breaking point’

On a recent day, a Dawsonville ambulance worker was trying to rush a patient with dangerously high blood pressure to the hospital.
But after a brief call, she learned its emergency department was on “diversion,” meaning her patient could wait more than an hour for a bed, tying up the ambulance from responding to other calls.
“I have been hung up ... and told to go else where!” she posted on the social media page of a statewide group of emergency medical personnel.
With every passing day of record-breaking COVID-19 infections, the severely overburdened hospital system is now stressing the backbone of the state’s emergency medical response system.
“I don’t know where our breaking point is, but I feel like we’re getting very close,” said Chad Black, director of the EMS Association of Georgia. “My concern is we have not (yet) seen the potential surge from Christmas and New Year’s. We have no capacity now, and if it gets worse, what do we do?”

So far, Georgia crews are continuing to transport every caller who dials 9-1-1. But after last week’s talk by Georgia hospital leaders of possibly needing to ration care to handle exploding cases, emergency medical services concede tough decisions may be ahead.
In other states with crippling hospitalizations, EMTs are having to transport only the most severely ill patients — and not take those who can’t be resuscitated.
Georgia crews fear they also may have to prioritize which patients to transport and which to leave behind. Troubling indicators are popping up all over the state, where dozens of ambulances are spending hours in the bays of crowded emergency rooms, waiting to drop off patients.
To relieve the pressure at some hospitals, physicians have taken the initiative to conduct examinations aboard the trucks. In rare cases, patients tired of waiting outside of ERs demanded to return to their homes, after losing hope that they will have access to a doctor. Habersham saw one such case only recently, Black said.
In the meantime, some emergency medical services have decided to staff ERs with their own paramedics to monitor patients until they can be admitted, freeing up ambulances to respond to other calls. Those being shifted to the ERs are typically older medics who have been performing administrative duties and no longer ride on the ambulances.
“The hospitals are full,’' said Steve Vincent, chief operating officer of Gold Cross EMS in Augusta, which is providing staff to ERs to help ease the overcrowding. “There’s no denying the wait times are getting a little longer.”
‘A weariness’
The challenges now facing crews are much greater than those during the pandemic’s onset.
In those days, most medics had not been exposed to the virus. Now, dozens have tested positive and have had to quarantine or become ill and had to be pulled off trucks in order to recover. Other medics pull long hours to fill in and keep ambulances running.
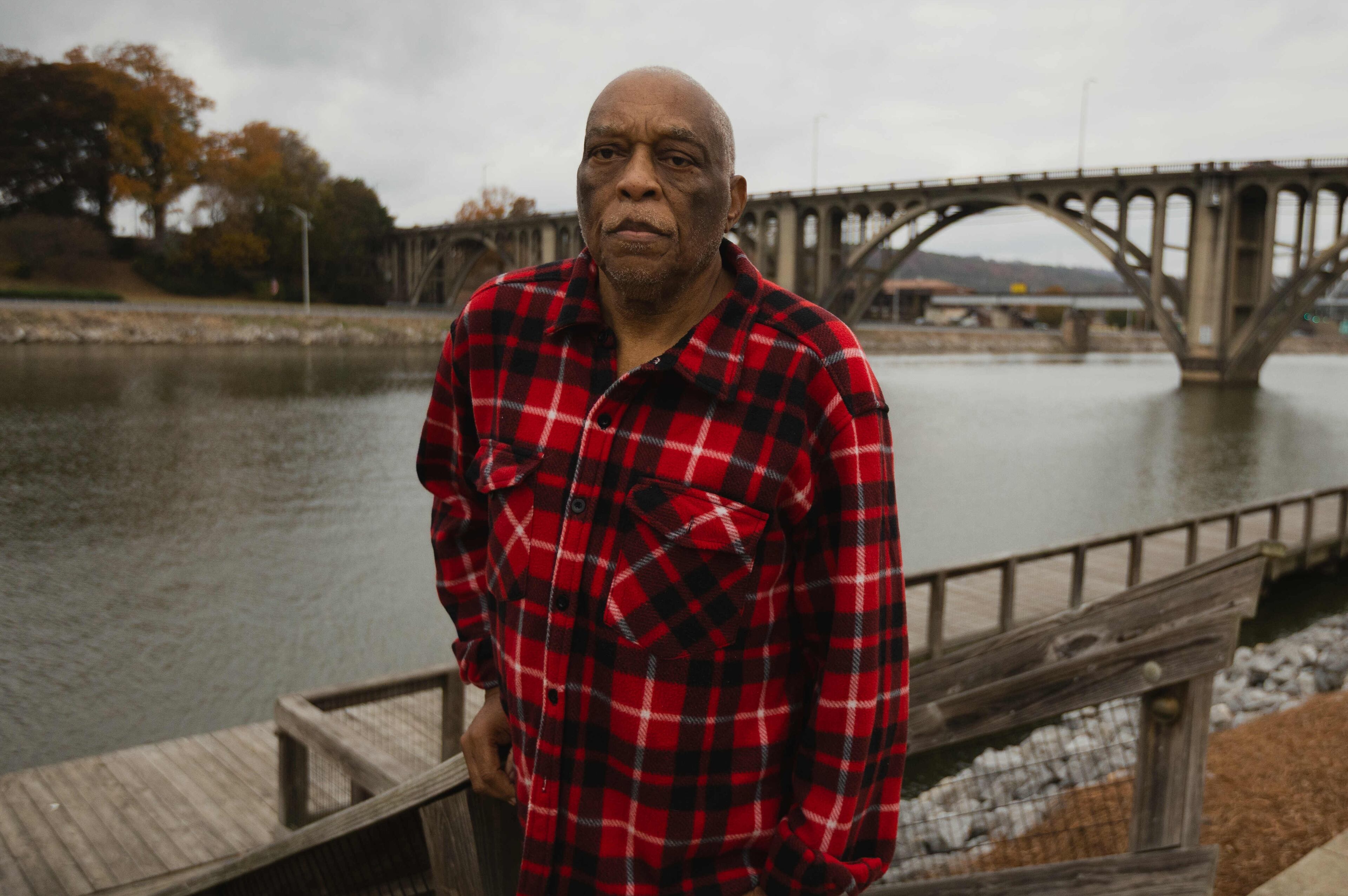
“Everybody is tired of it,’' Brantley County paramedic John Smith said. “It’s a weariness of a lot of the crews of working overtime.”
The loss of even a few medics can ground ambulances that are critical in a life-threatening emergency.
Black, who is director of Habersham EMS, has six trucks at his disposal. But on Monday, he only had enough medics to fill half. Several medics were out sick or under quarantine.
Meanwhile his call volume is exploding. In the hours that the three transports were running, the medics in the back of the ambulances ran a dozen more calls than usual.
“By the end, they are exhausted,’' Black said.

In east-central Georgia, EMS Director Blake Thompson has to transport patients as far as Athens and Augusta when no other facility is open for patients in need of critical care. That means one of his trucks is tied up for four to six hours before it can return to running calls in Wilkes County.
“When you tie up a truck for six hours, that’s unreal on rural EMS,’' Thompson said. “That’s a real problem. I need that truck back to run other calls.”
Not too long ago, some of his paramedics had to wait over four hours for a patient to be transferred to a bed at a hospital.
“I’m still raising hell about that,’' he said.
On diversion
To keep wait times for crews as short as possible, EMS depends on a statewide database that allows emergency rooms and ambulance services to communicate with each other.
Grady has a unique view of this database, called the Georgia Coordinating Center: In addition to operating a Level One trauma center and one of the state’s busiest emergency departments, Grady also has ambulance services in Fulton and other parts of Georgia.

“The GCC’s ability to direct ambulances and help hospitals balance patient loads is vital during these times of exceptionally high patient volumes,” the Grady administration told the Atlanta Journal-Constitution.
But, as hospitals reach capacity, it becomes a less handy communication tool for EMS to identify those hospitals that can best accommodate their patients.
Thursday evening, the database showed nearly three dozen emergency departments in hospitals in every corner of the state in a state of overcrowding, with more than two dozen in “severe” status. Those included major facilities in Metro Atlanta, including Grady Health System, Emory-Decatur Hospital, Wellstar AMC and Wellstar AMC South, as well as hospitals in Athens and Macon.
Before the pandemic, in northeast Georgia it was unusual to have multiple hospitals on “diversion” for days in a row, Black said. In recent weeks, it has become common.
“My understanding is that everything south of Gainesville is on diversion and now Gainesville is backing up,’' Black said. “It’s a domino effect.”
When a hospital is on emergency department diversion, that doesn’t mean that ambulance will be turned away, said Bobby McCullough, CEO of Memorial Satilla Health in Waycross, which had 44 COVID-19 patients but whose ER was not listed in “severely” overcrowded status as of Thursday.
For example, if an ambulance is trying to find a hospital with an open bed, the crew might learn from the database that it needs to travel longer distances to a hospital with one, in order to avoid long waits at a severely overcrowded ER that is closer.

“If we have a hospital 50 miles away and we’re on diversion and that hospital is not on diversion and it is not a critical patient who doesn’t require immediate care, we would ask our EMS partner to consider taking the patient to a facility that doesn’t have the same levels of holds or restrictions around their ability to admit patients,’' McCullough said.
A key point is that “diversion” does not signal to EMS that they cannot drop off patients, he said. “It doesn’t mean we’re closed,’' he said. “It doesn’t mean don’t come here. Just be thinking critically what is the best thing for the system.”
Workarounds
To try to keep as many ambulances on the streets as possible to respond to the most critical calls, Georgia EMS providers are using an assortment of initiatives.
Some have launched public awareness campaigns.
Many in the public, for example, do not understand that patients who arrive by ambulance don’t necessarily get to push to the front of the line compared to other patients waiting in the emergency department.
“Everybody is tired of it. It's a weariness of a lot of the crews of working overtime."
Just like every patient, the ones on an ambulance undergo a triage by clinicians, who then prioritize the immediacy of their care and level of treatment.
At Grady Health System, officials say they are relying heavily on their 10-bay ambulance triage area that allows it more capacity to bring patients directly from an ambulance to a room.
Last month, Barrow County Emergency Services issued a public notice urging callers to work with crews to help determine the best course of treatments.
“If a patient has mild symptoms, it may be in their best interests to stay at home and quarantine,’' Barrow officials told the AJC.
Chatham County has erected billboards to try to educate the public on how to seek more immediate care for a minor ailment at a clinic or urgent care center.
Chatham also is part of a federal pilot program that allows its medics to transport to patients with non-emergency conditions to urgent care centers and non-emergency rooms, said Chuck Kearns, CEO of Chatham Emergency Services in Savannah. Medicare, Medicaid and private insurance otherwise pay the ambulance bill only when a patient is taken to a hospital.
In some cases, Savannah paramedics also are trying to extend care to patients in their homes as a result of a program that enables them to negotiate with private insurance carriers a fee for service, Kearns said.
“We’re getting very creative as a means of necessity,’' Kearns said.