Federal funds aimed at easing front-line worker burnout, depression

At the peak of COVID-19 hospitalizations in Georgia, Dr. Deepak Aggarwal pulled into the driveway of the home he shares with his wife and two school-aged children.
In his years as a kidney doctor, the chief of the medical staff at Northeast Georgia Health System had never witnessed such a ruthless disease.
As was habit throughout the pandemic, he refrained from entering the house until he removed his clothes in the garage to avoid exposing his family. But on this day, just as the garage door opened, he saw his son dash outside to meet him. Behind the boy appeared his panicked wife, shouting: “Don’t touch him! Don’t touch him!”
“I have to take a shower and then I’m allowed to touch my kids,’' the physician said. “There’s that feeling in the back of your mind, that feeling of fear.”

Since the pandemic began over a year ago, thousands of front-line workers and first responders have been going to work each day – and carrying with them the fear of bringing home a deadly virus.
Now, as Georgia presumably enters the final leg of the threat, concerns are growing about the impact on the mental health of those who have lived through the worst, and whether they will have at their disposal the resources to address their psychological scars.
Over time, many front-line workers will ultimately suffer trauma-related disorders, such as anxiety and depression.
Experts say they will need to learn strategies for practicing self-care, including adopting physical exercise regimens. Some may need medications to ease their symptoms. Others will need group and cognitive behavior therapy, as well as Eye Movement and Desensitization Reprocessing therapy (EMDR), to process bottled-up emotions, mental health experts say. EMDR uses rapid eye movements and tapping exercises to aid in the processing of memories, which have triggered negative thoughts, feelings and behaviors.
So far, there hasn’t been a timetable released for how quickly the money will flow.
But the American Rescue Plan Act is expected to award grants to local governments, private and nonprofit organizations and health professions schools to develop strategies for reducing and addressing suicide, burnout, mental health conditions and substance abuse orders.
Physicians are twice as likely as the general population to die by suicide, national statistics show.
(Source: American Psychiatric Association, American Rescue Plan Act)
“They’ve yet to take a deep breath,’' said Dr. Matthew Norman, an Atlanta psychiatrist who has provided mental health services to Emory residents. “It’s only when you take a deep breath that you are able to recognize the toll of the stress and the strain of what has transpired.”
It could take months or even years for the traumas inflicted by the pandemic to surface, Norman added.
This spring, to address some of those concerns, Congress committed roughly $140 million to establish programs aimed at reducing suicide, burnout and substance abuse disorders among front-line workers.
The funding, under the American Rescue Plan Act, tasks the U.S. Health Resources and Services Administration with developing mental health and substance abuse disorder training.
Another part of the effort will analyze the scope of the problem and what it looks like.
Meanwhile, the Dr. Lorna Breen Health Care Provider Protection Act, named after a top emergency physician in Manhattan who died by suicide a year ago, prioritizes support for healthcare workers in COVID-19 hotspots in Georgia and other states.
“I’m hopeful that this funding will allow the proper health treatment to at least be available to front-line healthcare workers and others,’' said Norman, the Atlanta psychiatrist.
Lack of awareness
For years, front-line workers have had few places to turn to for help, and the state provided few options under a peer counseling program that lacked funding.
Efforts by a statewide committee of paramedics and EMTs also were stalled last spring after COVID-19 hit, which would have created the first statewide curriculum for treating those suffering from depression, burnout and Post-Traumatic Stress Disorder.
One obstacle to addressing mental health concerns during the pandemic is that little is known about how the nation’s healthcare providers and caretakers will react once the crisis is over, and how widespread the level of burnout and depression will be.
Another challenge is the mindset of many front-line workers, who despite the ease by which they are willing to lend help to others, are resistant to seek help for themselves.
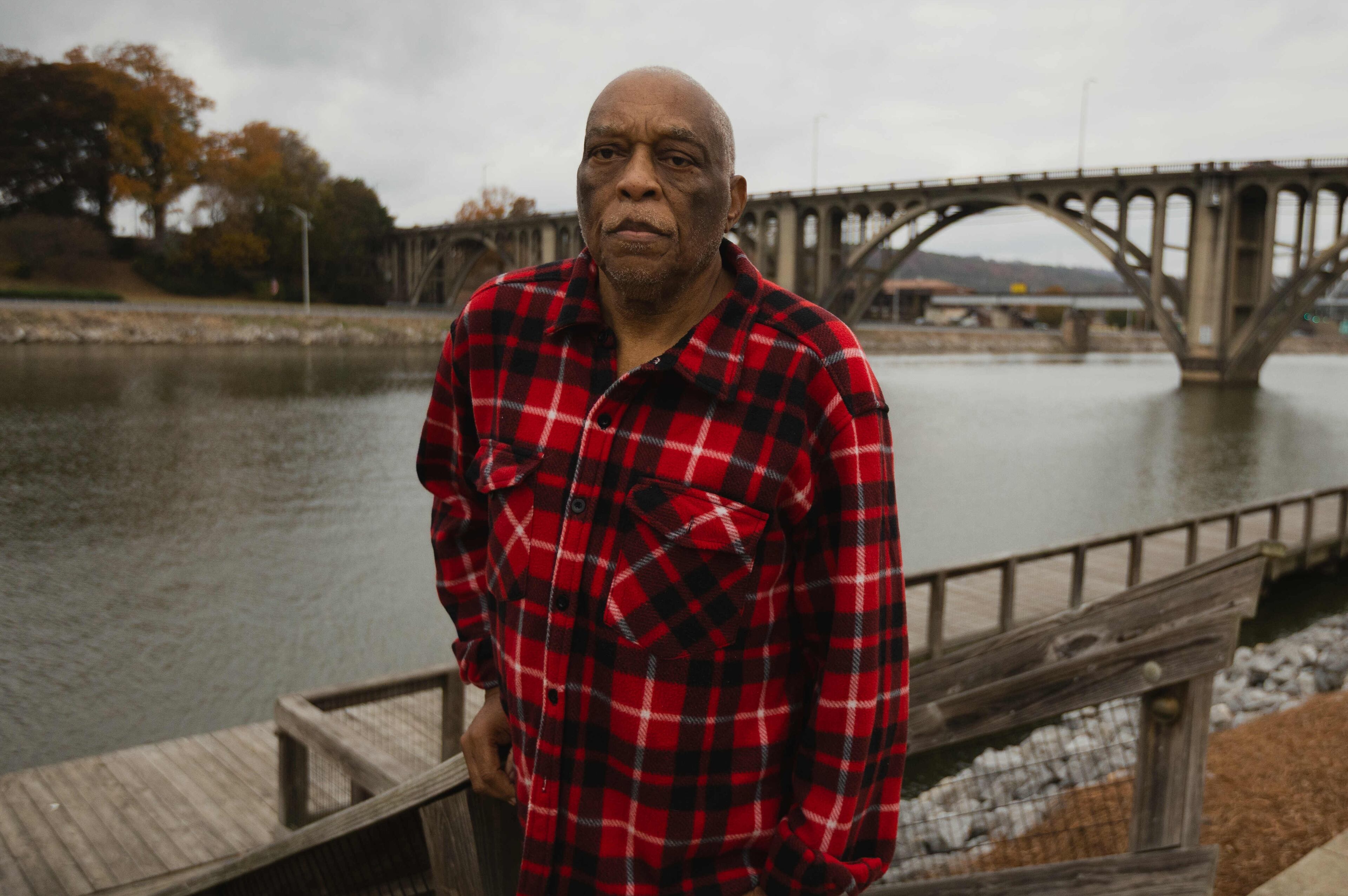
“We’re the rescuers,’' said Jeff Wilson, a retired Emergency Medical Technician and captain of the Atlanta Fire Department, who recently concluded a mental wellness program in Maryland for first responders. “We don’t feel like we need to be rescued.”
Flipping the switch
Kelly LaCerra rarely took breaks or had time to eat her lunch during the winter peak of the pandemic as a charge nurse in the ICU of a COVID-19 unit at Northeast Georgia Health System’s hospital in Gainesville. She was too busy running to medical emergencies at the facility, where hundreds died in the months of December and January.
At times, she and medical staff would spend up to two hours trying to revive a heart. “I’ve never worked so hard in my life,’' said LaCerra, who has been a nurse for more than three decades.
To do her job, she had to create an emotional distance between herself and her patients, she said.

It’s what front-line workers are taught to do to protect their mental health, said Molly Jones, a social worker and clinical outreach coordinator at the International Association of Fire Fighters Center of Excellence, a Maryland-based residential behavioral health program for emergency dispatchers and first responders.
That means they must be able to switch back and forth between their jobs and their personal lives, she said.
“If you aren’t able to flip that switch when you are at work, be present and emotionally armor up, you run the risk of becoming enmeshed with the people that you’re trying to help or you end up falling apart at work, and that’s not the healthy place to do that.”
A key part of mental health awareness is to be watchful for situations that become too personal, she said.
It also can be difficult to predict the timing of the manifestation of repetitive traumas. Unprocessed and difficult memories can surface as flashbacks and nightmares, which can trigger a fight or flight response, Jones said.
“They’re still seeing it, they haven’t even processed it yet, it’s still just swimming around in their brains right now and nothing really has been filed away,” Jones said. “My hope is that it will occur with more normalized perspectives and more resources.”

‘Bury it’
Wilson, 52, the Atlanta EMT-firefighter, found himself reliving a call that took place decades ago when he was a young EMT of 62-year-old twins who died instantly when a tractor-trailer rolled on top of their vehicle. An older sister who was riding in the backseat died several days later of related injuries, he said.
“These sisters, born on the same day, died exactly on the same day, at the same minute,’' said Wilson, who served with the Atlanta Fire Rescue Department for 28 years. “It was hard for me to process that emotion.”
He realized he had not fully processed the memory when he attended the program run by the International Association of Fire Fighters, he said.
“I didn’t know a lot of things were bothering me,’' he said. “In Maryland, it came out that this was really bothering me. It was hard for me to process that emotion.”
But back 30 years ago, when he started in the fire service, he was instructed to “bury it,” and be ready to respond to the next call, he said. “We didn’t deal with trauma. We were taught, ‘Hey, you got another call you need to push that aside.’”
Similarly, front-line workers haven’t had much time to reflect on the pandemic, and their traumas could surface many years from now, experts said.
“It is devastating and emotionally, it takes a big toll on all the providers because we’re just seeing so many deaths on a daily basis,” Aggrawal said. “You feel sad for the patients and their families. But you don’t get time to grieve because you have so many patients and so you just have to keep moving.”
Meanwhile, until there is some respite from the pandemic, it’s helped to share his thoughts with peers who are going through a similar emotional rollercoaster, he said.
“I have been voicing that more with our colleagues -- that we are all in this together,’' Aggrawal said. “It’s good to share your feelings so that you know everyone is going through the same experiences.”
NEW RELIEF DOLLARS: Where will the money go?
Over time, many front-line workers will ultimately suffer trauma-related disorders, such as anxiety and depression.
Experts say they will need to learn strategies for practicing self-care, including adopting physical exercise regimens. Some may need medications to ease their symptoms. Others will need group and cognitive behavior therapy, as well as Eye Movement and Desensitization Reprocessing therapy (EMDR), to process bottled-up emotions, mental health experts say. EMDR uses rapid eye movements and tapping exercises to aid in the processing of memories, which have triggered negative thoughts, feelings and behaviors.
So far, there hasn’t been a timetable released for how quickly the money will flow.
But the American Rescue Plan Act is expected to award grants to local governments, private and nonprofit organizations and health professions schools to develop strategies for reducing and addressing suicide, burnout, mental health conditions and substance abuse orders.
Physicians are twice as likely as the general population to die by suicide, national statistics show.
(Source: American Psychiatric Association, American Rescue Plan Act)