Physicians at Emory University Hospital performed the first-ever surgical implantation in the United States of a brand-new type of heart pump designed to help save patients with heart failure, using a smaller, more comfortable device.
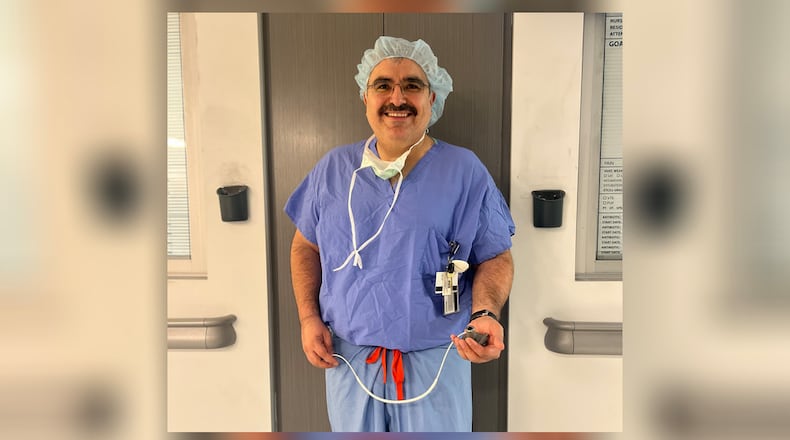
“It’s exciting to see innovation is still happening,” said Dr. Mani Daneshmand, an Emory cardiothoracic surgeon leading the clinical trial at Emory that is studying the new pump, known as a ventricular assist device, or VAD, with the brand name of BrioVAD System.
Daneshmand has worked with heart pumps for about 20 years. “We’ve gone from ‘How do we stop these people from dying?’, which is a high bar, but is also a low bar. Now, we’ve figured that how to stop them from dying. Now, let’s make them enjoy life more.”
VADs are mechanical pumps that are surgically implanted inside the chest to help the heart pump blood. The VAD can be a lifesaving treatment for patients with heart failure who are not responding to other treatments including medications, surgeries or a pacemaker. They can also serve as a bridge for patients waiting for a heart transplant.
Credit: custom
Credit: custom
Traditionally, VADs have been bulky and cumbersome, and they come with serious risks for complications, including infections at the site where the device’s cable exits the body. It requires major open-heart surgery to implant the device. The device is implanted inside the heart but has a controller unit and battery pack worn outside the body and connected to the VAD through a small opening in the skin.
Major improvements have been made in recent decades that allow people to live longer with fewer complications, and with a better quality of life compared to earlier versions of the device.
Daneshmand is hopeful the BrioVAD System will mark another major step forward in treatment. It has features designed to reduce complications and will be more comfortable to wear than earlier versions of the device.
After being authorized by the U.S. Food and Drug Administration to begin clinical trials earlier this year, Emory became the first site enrolled in the trial to use the BrioVAD System in a patient. As part of a clinical trial, Emory and other medical institutions across the country, including Cleveland Clinic Foundation, Duke University and University of Chicago, will track the safety and effectiveness of the BrioVAD System. They will compare the new device to other therapies on the market for treating end-stage heart failure.
The study will include about 750 patients over two to three years.
BrioVAD was developed by Massachusetts-based BrioHealth Solutions.
Credit: custom
Credit: custom
Daneshmand said the goal of the study is to show this product works about as well as standard treatments, and not necessarily better. Researchers will look for other important advantages, such as fewer side effects and ease of use and comfort.
Daneshmand said the BrioVAD pump is smaller than what’s currently commercially available, making it less cumbersome to implant and potentially less labor-intensive to remove if a VAD recipient needs a heart transplant down the line.
The VAD pump has a unique design, Daneshmand said, that mimics the natural rhythm of a human pulse while also being more gentle on the heart.
The wearable components are designed for patient experience, he said. The VAD that is available commercially now includes a controller and two large, heavy batteries, but the BrioVAD has a smaller controller with the backup battery included — meaning that the patient only needs to be hooked up to one, lighter battery.
“The design changes, I hope, are going to, in the long term, prove patients have less infection, less complications, and some things are practical. They don’t have to carry two big heavy batteries. They don’t have a big unwieldy driveline. They have a small flexible one. There is stuff the FDA doesn’t look into whether the patients prefer two batteries or one, but when we are taking care of patients, it does make a different for them, all of these things impact quality of life.”
An estimated 6.2 million Americans are currently living with heart failure — when your heart fails to pump blood as it should. Heart failure is responsible for 1 in 8 deaths in the U.S. per year, according to the Centers for Disease Control and Prevention. Recent data shows patients with advanced heart failure who receive a heart pump can survive five years and beyond.
Daneshmand said Emory Healthcare is leading the nation in implanting VADs, with physicians implanting between 80 and 100 of them every year.
Daneshmand said the patient who received the first BrioVAD System is in her early 30s, doing very well, and has been discharged. She has dilated cardiomyopathy, or DCM, a condition that causes the heart to enlarge and weaken, making it difficult to pump blood effectively.
As her health improves, she may be a candidate for a heart transplant down the road, he said.
“It is the most satisfying thing in the world to take someone who is sick and make them better,” he said. “There is no greater high than when a patient you saw who was sick and comes back and because of your team’s actions, they are better. ... She has an energy that is second to none. I think she will continue to do very well.”
Daneshmand said he has seen many iterations of the pump over the past two-plus decades.
He said what’s widely available today is great, but, “not perfect.”
“It’s an exciting time to be in this space,” he said. “The first iteration I ever worked with was a good pump for the time. It was something people could go home with and be supported but it was loud, it was noisy, reliably broke and patients needed multiple operations to be able to keep them alive,” he said.
About the Author
Keep Reading
The Latest
Featured