The Centers for Disease Control and Prevention officials said Thursday they still don’t know how a person in Missouri with no known exposures to animals or poultry recently contracted bird flu, but they don’t see any evidence of other people being infected and don’t see any evidence of person-to-person spread.
Last week, the CDC confirmed the 14th human case of bird flu in the U.S. this year. This latest case in Missouri, who was hospitalized on Aug. 22, was particularly concerning because there were no known contacts with infected animals or birds, sparking concerns over the possibility of human-to-human transmission of a serious virus that rarely infects humans. The patient recovered and was discharged.
However on Friday, a day after the press conference was held, the CDC issued more details on two other illnesses related to the Missouri case: “One household contact of the patient became ill with similar symptoms on the same day as the case, was not tested, and has since recovered. The simultaneous development of symptoms does not support person-to-person spread but suggests a common exposure. Also shared by Missouri, subsequently, a second close contact of the case – a health care worker – developed mild symptoms and tested negative for flu.”
The CDC noted a 10-day follow-up period has since passed, and no additional cases have been found. According to the CDC’s Friday report, “There is no epidemiologic evidence to support person-to-person transmission of H5 at this time.”
There never has been a confirmed human-to-human case of bird flu in the U.S. People have little to no immunity to this virus.
Mystery remains about the Missouri case. Missouri is not one of the 14 states that have reported outbreaks in dairy cattle, so it’s unclear how the human case there acquired the virus. The CDC confirmed on Friday it was able to determine that the H5 virus in the infected person in Missouri was H5N1, which is the type circulating in cows.
CDC Principal Deputy Director Nirav Shah said on Thursday that while epidemiologists have not found a clear source of exposure, they don’t see any evidence of spread of the virus between humans. He said the case appears to be a “one-off.”
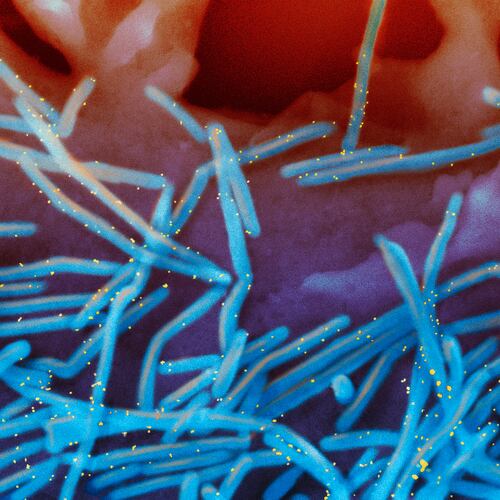
The bird flu has been spreading widely among wild birds, poultry, dairy cows and a growing number of other animals. Its rising presence in the environment increases the chances that people will be exposed and potentially catch it, Shah said.
While health officials wouldn’t reveal where in Missouri the case occurred, they have not seen any evidence of unusual levels of influenza activity in Missouri. There has been no increase in the volume of visits to emergency departments for influenza and no increase in laboratory detections of influenza cases in Missouri.
Shah noted unusual flu strains that come from animals occasionally are found in people. This year alone, health officials have identified seven human cases of swine flu in the U.S. But this is the first time the surveillance system detected an avian flu like this.
This version of bird flu — known as highly pathogenic avian influenza or by its scientific name of H5N1 — was discovered in a dairy farmworker April 1. That case marked the first time a human had caught the virus from a mammal. Since then, 13 people in the U.S. have been confirmed to have the virus.
Shah said the probe into the Missouri case continues and requires the work of “shoe-leather” epidemiologists. They are looking at whether the person visited a farm, a fair or a zoo, or had other potential exposures to animals. Was there contact with anyone who was sick? Was there consumption of raw dairy products?
CDC officials said the risk to the general public remains low. But they said they are continuing to look for changes in the virus that would change the agency’s risk assessment.
Georgia has not yet had a bird flu case associated with the growing outbreak in dairy cows.
Citing patient confidentiality, health officials have disclosed few details about the Missouri case, which was first announced late last week. The person had chest pain, nausea, vomiting, diarrhea and weakness, and was hospitalized Aug. 22 “for reasons related to their underlying medical conditions,” Shah said. The person has since recovered.
The patient was tested for flu as part of the treatment and was positive for influenza A, a broad virus category. Subsequent testing — completed last week — found the bug to belong to a category of viruses usually seen in birds and not people. But the patient had very low concentrations of viral genetic material, leaving officials without the ability to fully analyze and identify it, Shah said.
Shah also announced Thursday that the agency is working with five commercial companies — Aegis, ARUP, Gingko BioWorks, Labcorp and Quest — that make diagnostic tests to get them working on developing bird flu tests in case they’re needed in the future.
Seema Lakdawala, a virologist and influenza expert at Emory University, praised the commercial testing partnership, but noted, “That will only focus on humans.”
It’s not enough, she said. With this human case showing a link to the strain of the virus circulating in cattle but no cases among cattle herds in Missouri, she said, “This suggests something is missing here.”
Without routine testing at dairy farms, she said it’s likely cases are being missed. She called on the USDA to form partnerships on cows “to get more granular information about the extent of this outbreak and how widespread it is.”
The Associated Press contributed to this article.
Editor’s Note: This story has been updated to reflect new information released Sept. 13 by the CDC concerning contacts of the Missouri case who were also reported to be sick at the same time. The agency also confirmed that the virus the Missouri case had was H5N1.
About the Author
Keep Reading
The Latest
Featured